From Healthy to Helpless to Hopeful: My Life With Post-COVID POTS
Written by Alexandria Yarborough, PharmD
What if your health and life as you knew it turned upside down, and you could not figure out why? That is exactly what happened to me and the 6-7 million people who have been newly diagnosed with Postural Orthostatic Tachycardia Syndrome (POTS), since the COVID-19 pandemic hit the United States in 2020. Before then, about 2 million people were living with this life-changing condition.
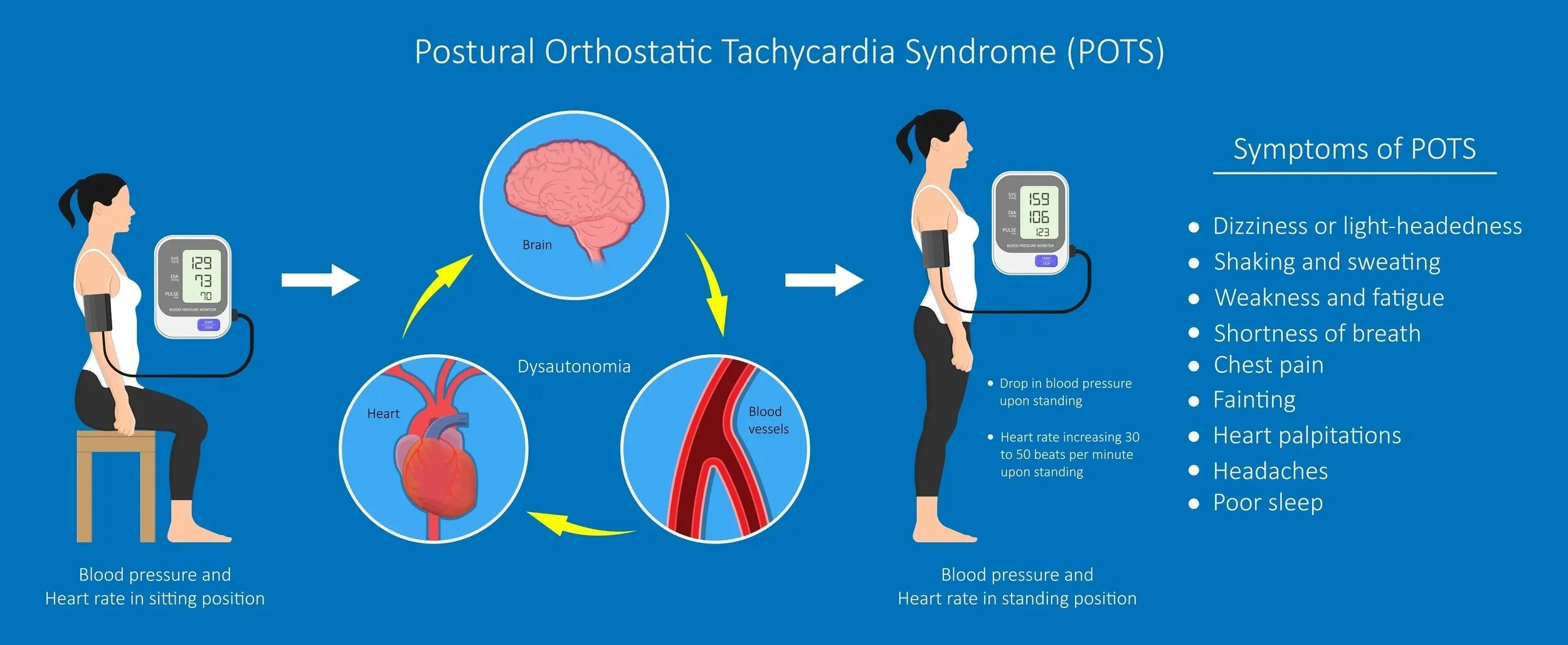
A simple definition describes POTS as dysregulation of the autonomic nervous system or dysautonomia. Personally, it feels as if some of my systems that are usually normal for everyone else malfunction without any triggers or any explanation.
My story unknowingly began in 2020, before the vaccine was available, and I caught a severe case of COVID. At that time, there wasn’t much you could do beyond supportive care. I was out of work for almost 2 weeks, but I thankfully recovered.
A few months later, I started having severe chronic fatigue, and my body felt as if I was running hot. It wasn’t necessarily a hot flash, and I didn’t feel sweaty. For instance, if I vacuumed a rug, I would become exhausted and feel extremely flushed. It was complete temperature dysregulation. I was never cold despite it being chilly outside. I couldn’t use blankets or jackets the same way I had most of my life.
Months later, I started having sleep issues – trouble falling and staying asleep. If I did sleep 6-8 hours, I would wake up feeling as if I hadn’t rested at all. Two years later, my heart rate started increasing. My symptoms increased gradually. It started with fatigue, temperature dysregulation, and sleep issues, and once my heart rate was uncontrolled, I knew something was off.
It was hard to explain at the time because some days I was perfectly fine, and other days were debilitating. I might feel only fatigued one day, but have a myriad of symptoms the next. My symptoms might last for a whole day or just a few hours. It was increasingly frustrating to understand what was going on with my body.
Once my heart rate issues began, the biggest impact on my life appeared. I could no longer exercise. I wasn’t able to stand and cook a meal. I no longer had the energy to do some of my crafts and activities. It was just really interfering with all aspects of my life. I have ADHD and once my heart rate became unpredictable, I was no longer able to take my ADHD medication because it’s known to increase heart rate. Not being on that medication resulted in increased brain fog.
Most POTS patients do experience fainting or almost fainting (pre-syncope). I had a few instances of pre-syncope, but thankfully not as many as other patients do. At times, I experienced numbness or tingling in my hands and feet. I was often nauseous or had no appetite at all. It was hard to have all of these unexplained symptoms and not know what to do, especially because there were so many different areas of my body not cooperating.
What is POTS?
The Cleveland Clinic defines POTS as “a condition that causes your heart to beat faster than normal when you transition from sitting or lying down to standing up.”
Each word of “postural orthostatic tachycardia syndrome” has a meaning:
Postural: the position of your body.
Orthostatic: standing upright.
Tachycardia: heart rate over 100 beats per minute.
Syndrome: symptoms that happen together.
Normally, your body’s autonomic nervous system balances your heart rate and blood pressure to keep your blood flowing at a normal rate no matter what position your body is in. If you have POTS, your body can’t coordinate the balancing act of blood vessel constriction and heart rate response. This means that your body can’t keep your blood pressure or heart rate steady and stable. Each case of POTS is different because every person is different!
Finding Answers in the Chaos: My Long Road to a POTS Diagnosis
I will preface my diagnosis story by saying it was rather quick for someone with POTS. I received my diagnosis in 2023, about six to eight months after I first went to my primary care provider. I am so thankful that she was empathetic. I really felt as if she listened to me. I did, however, not go to my appointment empty-handed. Since my symptoms were inconsistent and varied, I decided to track my health data
Once my heart rate started to increase, I bought an Apple Watch so it could monitor my heart rate throughout the day and when I felt it racing. I wanted to reassure myself that what I was feeling was actually happening to my body. I also took notes of what I was doing, such as walking up stairs or simply sitting down, to show that the spikes were random and not correlated with exercise or an explanation that would be brushed off.
While it was helpful to have my own health data, my doctor also had to obtain her own. She sent me home for 3 days with a Holter monitor, a small, wearable device that records the heart's rhythm. It's used to spot irregular heartbeats and heart rates. Thankfully, that health metric allowed her to see that something wasn’t right. She referred me to a cardiologist.
From getting a referral to the actual appointment took time. I first had an appointment for an ultrasound of my heart to make sure that there were no issues with the structure and function; there were none identified. I asked for a tilt table test, which is performed in patients to find out why certain patients become dizzy or faint. Unfortunately, my insurance didn’t cover it, so my cardiologist went a different route.
I was given an event monitor. It’s a type of heart monitor that sticks on your chest and is worn for 2-4 weeks. Anytime I would feel my heart rate increasing, I would press a button on an accompanying device to track an “event”. It would also record any spikes in heart rate throughout the day. Thankfully, the event monitor outcomes mirrored the Holter monitor results, and my cardiologist was able to use that data, combined with my symptoms, to give me a diagnosis of POTS.
I also had to visit other specialists who were not directly related to my POTS. I was referred to see a sleep medicine specialist, where I had an at-home sleep study and an inpatient one. Once those results were available, I was diagnosed with idiopathic hypersomnia, which is a fancy way of saying, we don’t know where this comes from (idiopathic) and hypersomnia, which is extreme daytime sleepiness. I was then prescribed a liquid sleep medicine that I have to take each evening in order to fall asleep and rest.
At one point, I went to my OB-GYN to switch contraceptive methods, just to make sure that my “running hot” wasn’t hormonal or a side effect from my IUD. It was challenging to try to navigate numerous appointments, insurance, and work schedule, on top of not feeling well.
Learning to Speak Up—Even When I Felt Silenced by Symptoms
I am thankful that I had an excellent experience obtaining a diagnosis. I do think that my healthcare background was helpful in that regard. I am a pharmacist, and my primary care physician knew that before my symptoms started. I don’t immediately mention my profession at doctors’ appointments, but usually divulge it when they inquire about medications. I think the only advantage of being a pharmacist with POTS is knowing more than the average patient about how complicated the healthcare system is. I am more knowledgeable concerning appointments/referrals, medication approvals, prior authorizations, time to diagnosis, etc., because it is a part of my day-to-day job.
The biggest tip I can tell anyone, whether they are in the healthcare field or not, is to document. It would have been extremely hard for my physician to hear the number of symptoms I was having and know where to begin addressing issues. Since I had the heart rate data from my Apple Watch, she was able to refer me to a cardiologist. Because I provided a journal documenting my sleep issues, she was able to refer me to a sleep medicine specialist. Documenting your symptoms and tracking health data can be tedious, but it can really help your providers make informed decisions concerning your health.
Advocacy is hard, especially when you aren’t feeling well and you no longer feel as if you have control over your body. As much as I would like to have used my healthcare background to expedite the process, I still had to go through the same steps as everyone else.
The Myths That Hurt: What People Get Wrong About POTS
There are a lot of misconceptions about how to manage POTS. One of the most common is that POTS can be cured with exercise. Because of this, friends, family, and providers with little knowledge of treating POTS patients may recommend that you exercise to improve symptoms. That may be an option for some patients in certain circumstances. For me, if I am feeling well, I might try to walk on a treadmill or take my dogs on a stroll.
However, if you aren’t feeling great, DO NOT push yourself. Exercising can exacerbate your symptoms and make you feel worse if you overexert yourself. I always listen to and am kind to my body. Even if I am feeling well and get a walk in, I am reasonable with my expectations.
Another common misconception is that POTS is “all in your head.” Technically, that is true. Your autonomic nervous system is controlled by an area of your brain called the hypothalamus. Despite truly being controlled by your brain, POTS is not a mental condition. It is a dysregulation of the nervous system throughout your body. It can not be cured by the power of positive thinking or overcome by willpower. It is very much a real illness that requires a healthcare team, medications, etc.
Why the Healthcare System Needs to Catch Up on POTS
I would love to see changes in the healthcare system when it comes to managing POTS. Even though I am thankful to my providers for the empathy and understanding they showed with my condition and how they believed my experience, it was difficult to arrive at a diagnosis.
Our healthcare system needs to shift from treating symptoms to treating the whole patient. I was experiencing issues with sleep, my heart, fatigue, and other body systems. I was offered medication for each one. Some were necessary, others were not. I think it’s important to focus on a patient’s overall health and what lifestyle changes, medication regimens, and wellness options are available to them. In my experience, there needs to be short-term and long-term goals.
POTS is a hard condition to navigate. It would be helpful to look at the issues that are affecting us day-to-day and then help us plan for what they will look like in the future. In my treatment, the first issue to tackle was sleep. Once I was sleeping well, we focused on my heart rate.
I was given: a daily extended-release maintenance medication and an as-needed immediate-release medication for my heart rate. In the beginning, I used the immediate-release medication a lot. Now that I am on the correct dose of the extended-release medication, I rarely need the immediate release.
This type of success can only be achieved with collaboration. It can be confusing and frustrating to have a different specialist for your heart, sleep, and your primary care provider. It takes a team to manage POTS, and this only helps make collaboration and treatment easier.
Alex, who is a huge Harry Potter fan on a trip at Universal Studios Harry Potter World.
What POTS Taught Me About Strength, Gratitude, and Self-Advocacy
POTS taught me how resilient I am. I never thought a chronic condition would happen to me. I was a healthy 28-year-old before my diagnosis. It’s made me extremely grateful for my health. I now realize that life can change in an instant. Because of that, I encourage everyone to practice gratitude. I have learned that you can’t buy good health. There is no special fix-all medication, new doctor, or any type of exercise that you can do just to make this condition go away. No one is going to save you; you must be your own advocate.
The biggest piece of advice I can give to someone experiencing POTS symptoms is to document. It can be as simple as a printed calendar with notes such as: little sleep, HR up, tired, etc. Doctor's appointments can take weeks or months; it’ll only help you if you are able to provide detailed information about what symptoms you are experiencing over time. Data is how decisions are made and will only help you on your journey to diagnosis.
Keep learning about POTS and hear more from Dr. Alexandria Yarborough by checking out the YMyHealth podcast on our YouTube channel or your favorite streaming platform!