Surviving Young Onset Colorectal Cancer: Allison Rosen's Story
Written by Melissa Schenkman, MPH, MSJ
In this exclusive Q&A, we speak with Allison Rosen, a 13-year survivor of early age onset colorectal cancer, Director of Project ECHO at the American Cancer Society, and dedicated patient advocate. Diagnosed at just 32 years old, Allison shares her unexpected journey through diagnosis, treatment, and how she transformed her personal experience into a mission to educate and advocate for others.
Before your diagnosis, what did you know about colorectal cancer?
Rosen: I worked in research, specifically in blood cancer, but I really had no idea about colorectal cancer. Like a lot of people think nowadays, I thought it was an old man's disease. I had no idea I was at risk or that I could get it. I didn't really know the signs and symptoms. I did have a history of digestive issues, so I knew my body, but colorectal cancer was the last thing on my mind.
What symptoms led you to seek medical attention?
I experienced several symptoms that are pretty typical for colorectal cancer: blood in my stool, unexpected weight loss (which I initially attributed to doing Zumba 5-6 times a week), and severe fatigue. There was also a change in bowel habits, but what really concerned me was that when I would eat, it felt like something was getting stuck inside me. I'd have pain, and it felt like the food wasn't moving through my system. It got so severe that I talked to my doctor, who moved up a colonoscopy I already had scheduled. The colonoscopy revealed a 13-centimeter tumor blocking my colon.
How did you learn about your diagnosis, and what was your initial reaction?
A few days after my colonoscopy, my doctor called and asked me to come to her office. Since she had previously said, "I don't think it's cancer," I immediately knew something was wrong. I walked over on the phone with my mom, crying because I sensed bad news was coming.
In her office, she told me I had colorectal cancer, though she didn't know what stage yet. She mentioned potential inflammation in my lymph nodes and said I needed to find an oncologist and surgeon as soon as possible. Then she left me alone to process the news.
My life flashed before my eyes. I called my friend from the lab to get my keys and car because I wasn't ready to tell anyone else. Then I called my mom, who's a breast cancer survivor herself. When I went to her house, she said, "I wish it was me," and I told her, "I'm young. Besides the cancer, I feel like I'm healthy. We can do this. I need you and dad to be my caregivers and help me."
What treatment options were presented to you?
Because I worked in research in Houston's medical center, I knew people at MD Anderson, Methodist, and Baylor. I sought multiple opinions but ultimately chose MD Anderson because the oncologist there told me, "You're not just a number. I want to make sure that you get the treatment that's right for you."
Back in 2012, the standard treatment was radiation and chemotherapy, followed by surgery, and then more chemotherapy afterward. I would go for radiation every day after work at 5:30 pm since my lab was in a building across from MD Anderson. During the last two weeks, my mom had to pick me up because the radiation really takes a toll on your body.
Initially, they thought I was stage three, but after scans, they determined I was stage two C. I had surgery for a colon resection and received a temporary ileostomy. However, I experienced numerous issues with inflammation and infections afterward. I had a J-pouch created (an internal pouch), which they don't do as much anymore. After multiple hospitalizations for infections, I needed another ileostomy.
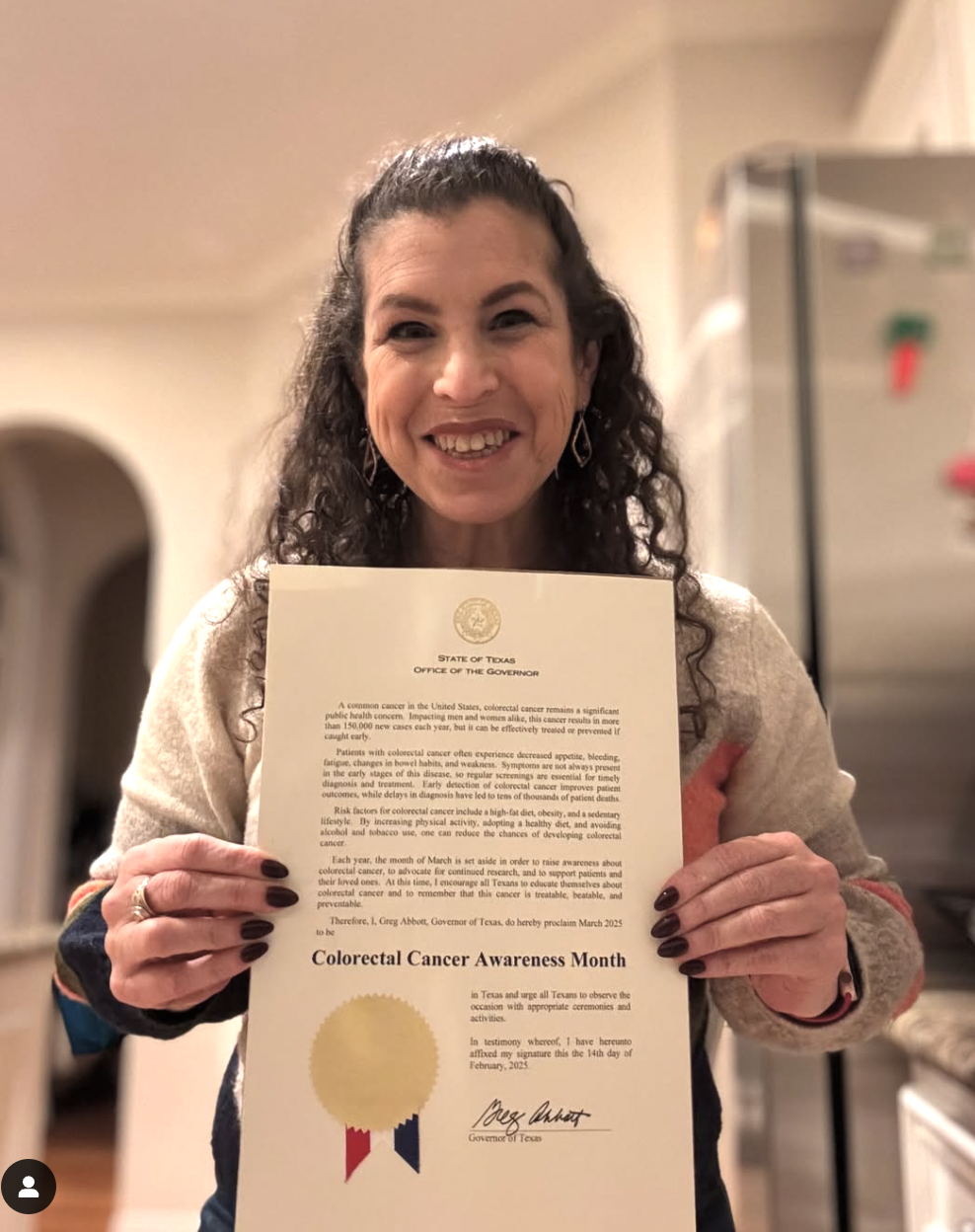
Allison proudly holding her state of Texas 2025 proclamation that the month of March is Colorectal Cancer Awareness Month.
You now have a permanent ostomy. How did you come to that decision?
After two years with a temporary ileostomy, I had an honest conversation with my surgeon. He said we could try another reversal, but I might continue to have lower anterior resection syndrome or more infections.
By then, I had gotten used to the ostomy. My quality of life had improved, I'd gained weight, and I was able to eat what I wanted. We decided together that for quality of life and to prevent colorectal cancer recurrence, a permanent ostomy was best. I've had "Phil," my ostomy, for about 8-9 years now, and I'm doing great.
What resources did you find for young-onset colorectal cancer patients, and how have you seen that landscape change?
It's changed tremendously. When you're sitting in a GI clinic as a young person, you look around and everyone's much older. MD Anderson had a program for adolescent young adults (AYAs), which was mostly social. I attended an event at the zoo where I met other young adult cancer patients. Although none had colorectal cancer, it was amazing to connect with people who understood my experience. I later joined their AYA advisory council.
I also searched online for "colorectal cancer support Houston" and found the Colon Cancer Coalition. They had a race, and when friends and family asked how they could help, I invited them to participate. I'm now the director of that race and have been for about eight years.
I became involved with multiple organizations to learn about available resources and to help others. I joined Fight CRC's RATS (Research Advocacy Training and Support) program and have been a "rat" for about eight years. I also connected with the Colorectal Cancer Alliance's "Never Too Young" initiative.
Through these organizations, I've learned about resources for transportation, financial support, fertility assistance, and psychosocial support. Being involved has allowed me to help others navigate their cancer journeys.
What motivated you to transition from cancer research to public health and advocacy?
I've always been a learner and have always wanted to help people. I volunteered since childhood at the children's museum and zoo. When I got involved in cancer advocacy, I received so much support that I wanted to dedicate my career, both inside and outside of work, to helping others.
Having worked in research and gone through the cancer journey myself, my goal has been to bridge the gap between these worlds. Researchers often work in silos, and I realized how valuable it would be for them to have access to survivors who could share the real effects of cancer treatments.
After several years of having no evidence of disease, I moved into public health. My goal is to educate people in the community about the importance of screening and early detection, while also educating healthcare providers, clinicians, nurses, community health workers, and social workers. I believe everyone needs to work together to advance research, education, and awareness.
Want to hear more from Allison Rosen? Check out the YMyHealth podcast on our YouTube channel or your favorite streaming platform!